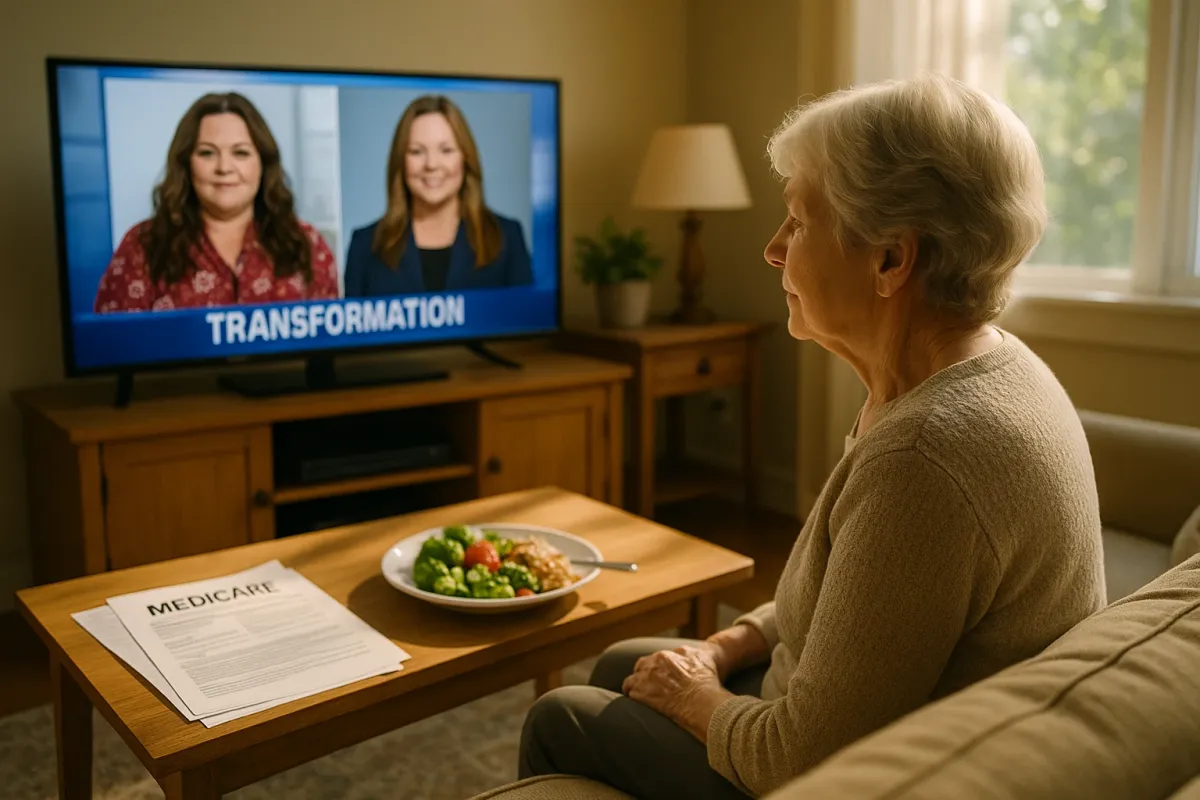
Melissa McCarthy’s recent 95‑pound weight loss has ignited a storm of speculation—especially after her buzz‑worthy “SNL” appearance and Barbra Streisand’s very public question about whether weight‑loss injections were involved. It is the kind of viral moment that blurs the line between inspiration and pressure, between genuine health improvement and Hollywood illusion. For adults navigating weight, aging, and Medicare, the conversation looks very different from a red‑carpet reveal—yet the health benefits at stake are far more enduring than a single trending clip.
Behind the celebrity headlines lies a quieter, more consequential story: sustained weight reduction in older adults can lower cardiovascular risk, improve mobility, protect independence, and enhance quality of life. But the path to those benefits must be medically sound, metabolically appropriate for age, and aligned with coverage realities. Using McCarthy’s transformation as a timely lens—without attempting to copy or second‑guess her private choices—let’s examine what truly elevated, evidence‑based weight management can look like for Medicare beneficiaries today.
1. The Real Health Dividend of “Steady, Not Spectacular” Weight Loss
Viral celebrity transformations often appear overnight, but the most powerful health benefits for older adults accrue from gradual, clinically supervised weight loss. Research shows that a sustained 5–10% reduction in body weight can lower blood pressure, improve cholesterol, reduce sleep apnea severity, and meaningfully decrease the risk of type 2 diabetes progression—benefits that matter far more than hitting a dramatic number on the scale.
For Medicare beneficiaries, this nuance is critical. Rapid, extreme loss can mean unintended muscle wasting, worsened frailty, and higher fall risk—especially for those over 65. The gold standard is a tempo that allows your cardiovascular system, joints, and metabolism to adjust gracefully. A carefully designed program might target 1–2 pounds per week early on, tapering as you approach a sustainable weight range. While social media fixates on “before-and-after,” your physician will be more interested in reductions in A1C, improvements in gait speed, and whether you can climb a flight of stairs without stopping. Those are the quiet metrics that forecast independence in your 70s and 80s.
2. GLP‑1s, Ozempic Buzz, and How to Judge Whether Advanced Therapies Fit Your Profile
The speculation around McCarthy’s weight loss reflects a broader cultural obsession: GLP‑1–based medications such as semaglutide and tirzepatide, sold under brands like Ozempic, Wegovy, and Mounjaro. These drugs can be powerful tools for certain patients with obesity and metabolic disease, and they are increasingly entering Medicare conversations. Yet they are not a universal solution—and certainly not a substitute for medical judgment.
For Medicare beneficiaries, the key question is not, “Did a celebrity use an injection?” but rather, “Would this class of medications be safe and appropriate for my specific risk profile?” A refined evaluation includes kidney function, history of pancreatitis, current medications, cognitive status, and your ability to maintain lifestyle adjustments that enhance and stabilize the drug’s effects. GLP‑1s can reduce appetite and facilitate significant weight loss, but in older adults they must be paired with strategies that protect lean muscle and bone density. Engaging a physician who understands both obesity medicine and geriatric nuances is essential; this is not a prescription to request simply because a headline suggests it is fashionable.
3. Protecting Muscle as You Lose Fat: The Overlooked Luxury of Functional Strength
In celebrity narratives, the spotlight is on dress size and camera angles; in Medicare‑age medicine, the true luxury is preserved strength, balance, and resilience. After age 50, adults naturally lose muscle mass each decade—a process amplified by unstructured dieting and rapid weight loss. For every 10 pounds you shed, you want the vast majority to be fat mass, not hard‑earned muscle.
A premium, health‑focused weight program for older adults should include: objective baseline measurements (weight, waist circumference, and when possible, body composition), a protein plan calibrated to your kidney health (often 1.0–1.2 grams of protein per kilogram of body weight for many older adults, customized by your clinician), and strength‑focused movement—resistance bands, light free weights, or chair‑based exercises tailored to joint health and cardiovascular status. Medicare beneficiaries sometimes underestimate how transformative modest strength gains can be: standing up from low chairs without bracing, carrying groceries without back pain, navigating curbs confidently. While the internet debates whether a celebrity “cheated” with injections, your more sophisticated win is a body that remains capable, not just thinner.
4. Emotional Narratives vs. Objective Health: How to Watch Celebrity Stories Without Internalizing Them
Public reactions to McCarthy’s transformation have ranged from effusive praise to suspicion and shaming—reminders that weight remains one of our most emotionally charged topics. For older adults, especially those who have dieted for decades, such stories can trigger frustration (“Why is it so easy for them?”) or urgency (“I need something drastic now”). Both reactions can lead to hasty, unsafe choices.
A refined approach is to treat celebrity transformations as conversation starters, not blueprints. Ask: What health outcomes do I actually care about—lower cardiovascular risk, fewer medications, better sleep, improved energy? Which metrics can I track objectively with my physician—blood pressure, A1C, lipid panel, step count—not simply the bathroom scale? And which aspects of my relationship with food, movement, and body image deserve quiet, compassionate attention, perhaps with a therapist or health coach? Medicare may not cover every supportive service, but integrating psychological support—whether through covered behavioral health visits or reputable community resources—often determines whether weight loss becomes a sustainable, health‑enhancing shift or another cycle of regain.
5. Elevating Your Own “Program”: Coordinating Medicare Benefits for a Truly Integrated Plan
Behind every glamorous transformation sits an infrastructure—trainers, chefs, physicians, stylists. While that level of support may be unrealistic, Medicare beneficiaries have access to a surprisingly robust toolkit that, when elegantly coordinated, can approximate a structured “program” focused on genuine health benefits.
Key elements include using your Annual Wellness Visit to explicitly address weight, mobility, and fall risk; exploring coverage for intensive behavioral therapy for obesity when medically appropriate; clarifying whether your plan offers nutrition counseling for diabetes, kidney disease, or post‑cardiac events; using supplemental benefits (in many Medicare Advantage plans) for fitness programs or gym memberships that include senior‑friendly strength and balance classes; and documenting comorbidities—hypertension, prediabetes, sleep apnea—with precision, as this often influences eligibility for advanced therapies, including certain anti‑obesity medications when and where they become covered. The more organized and medically documented your history, the easier it is for your clinician to justify comprehensive interventions that meaningfully improve long‑term health, not just weight.
Conclusion
Melissa McCarthy’s striking transformation has captured the public imagination, but the more consequential story for Medicare beneficiaries is not how a celebrity changed her silhouette—it is how you can thoughtfully reshape your health trajectory in your 60s, 70s, and beyond. The true privilege is not rapid, camera‑ready weight loss; it is a heart that works less frantically, joints that carry you without protest, and a body that remains a reliable partner in the life you still want to lead.
By prioritizing steady loss over spectacle, evaluating medications with clinical nuance, protecting muscle, disentangling your self‑worth from headlines, and orchestrating your Medicare benefits into a coherent plan, you transform weight management from a trend‑driven chase into a sophisticated, health‑first strategy. Celebrity moments will come and go; the health benefits of well‑managed weight, especially in later life, are designed to stay.
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Health Benefits.